


Hip replacement has been among those operations that has earned immense success in the medical field due to minor complications and speedy recuperation rates.
The method that orthopaedic surgeons employ is known as anterior hip replacement, one among numerous less invasive surgical procedures that are linked to briefer hospitalization, smaller-sized slit, lesser muscle injury, less painfulness and bleeding, lesser chances of the hip dislocating post-surgery, swifter recuperation and a faster revert to normal existence.
Patients have cited being capable of walking with no need of walkers or canes and being capable of putting complete weight on their operated side. Within a day’s time post-surgery, patients are discharged from hospital and are able to walk home sans any limping. An exhaustive physical therapy is to be followed by such patients recommended five times per week for a fortnight that they could do in the confines of their home.
A specially designed operating table was developed for simplifying the method. The PATH method is another least invasive kind of hip replacement created by a LA orthopaedic surgeon Dr. Brad L. Penenberg that has analogous benefits as that of the fore strategy, resulting in no form of restrictions in movements and additionally offering a safety shield of repairing any aspect going erroneous during the method being resolved with not need to perform a further extensive surgery.
 A nearly two-decades-old surgery in the U.S. has become increasingly popular with almost two lakh hip replacement surgeries being conducted annually, with figures growing continually as the populace shows signs of aging. There are no age constraints for this optional surgery except when a causal health condition would make any surgery too perilous.
A nearly two-decades-old surgery in the U.S. has become increasingly popular with almost two lakh hip replacement surgeries being conducted annually, with figures growing continually as the populace shows signs of aging. There are no age constraints for this optional surgery except when a causal health condition would make any surgery too perilous.
The common grounds for hip replacement are rheumatoid arthritis (RA), osteoarthritis, hip fracture and painful arthritis that could cause pain and rigidity thus limiting a person’s motility and capability of performing day-to-day tasks. Majority of the patients attempt lesser radical measures – physiotherapy, drugs (pain allayers, inflammation-combating medicines and glucosamine supplemental forms), hyaluronic acid shots and walking supports – prior to arriving at the decision that surgical procedure is their best shot for evading unremitting pains and disablement.
To realize the prospective advantages of least invasive procedures, it would help to discern the manner in which hip replacement is performed.
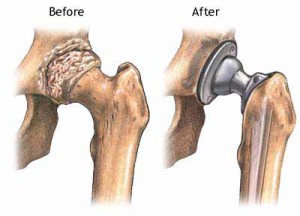
Prior to surgery, the patient is anaesthetized (general or spinal) that classically ensues for 1-2 hours. A ten to twelve inch long slit is done via the muscles on the hip side for exposing the hip joint, and the ailing bone tissue and gristle are excised. Implantation of a synthetic socket is then done into the pelvic bone and insertion of metallic stem is done in the thigh bone, the top-part of which is changed to a metal ball for creating a ball-socket joint which ably imitates the functionality of an innate hip joint.
The standard hospitalization time period is 4-5 days, mostly subsequent to which wide-ranging physiotherapy is done. Certain precautions are advised like not crossing legs or bending at the hip more than a perpendicular angle following surgical procedure – in few scenarios these safety measures have to be followed life-long, as such movements could lead to the hip replacement dislocating requiring another procedure to be re-done.
Likely post-surgery complications include formation of blood clot, infections, fractures and a variation in length of the leg. Likely late complications comprise of a dislocated newly replaced joint, fracture or disengagement of the artificial implant and rigidity of the tissues placed adjacent to the joint. Despite current materials being employed that have lengthened lifespan of implants to nearly two decades; however they could ultimately face wear and tear and hence need to be replaced.
The following post-surgery restrictions that all patients must be sentient about regarding these home amendments:
Researches evaluating long-standing outcomes of least invasive hip replacement with more conventional surgery have had sundry outcomes, and all types of hip replacements have garnered benefits from enhanced anaesthetic and pain allaying methods. Those performing surgeries regularly employing least invasive techniques assert that there are decisive benefits in majority of the patients, although the surgery on its own could be lengthier.
Conceivably, highly significant aspect is that chief muscles in the butt and thighs which aid in stabilizing hip joints are not severed, lowering the chances of dislodgment and swifter convalescence, briefer hospitalization and returning sooner to normal tasks.
As gaining adeptness in performing complex hip replacements is directly proportional to the number of operations performed by the surgeon, it is imperative that the surgeon’s work experience credentials be queried prior to deciding on the surgeon.
Irrespective of the form of surgery, it is helpful for patients to own supporting muscle sets as sturdy as doable prior to operation, perchance via numerous physiotherapy sessions in case the patient’s health state permits it.